What is a Spermatocele?
Spermatocele is a fluid-filled cyst that develops in the epididymis that is inside the scrotum. The epididymis is the tube that collects and transports sperm from the testicles. This common condition is usually noncancerous and painless, although it can cause discomfort and even require surgery if it grows large enough.
Symptoms of spermatocele may include a painless lump or swelling in the scrotum. It may also cause a feeling of heaviness or discomfort in the affected area. While it is not typically a serious condition, it is important to seek medical attention if you experience any of these symptoms or have concerns about your reproductive health.
In this article, we will explore the causes, symptoms, diagnosis, and treatment options for spermatocele. We will also discuss the potential complications and prevention methods for this condition. By understanding more about spermatocele, you can take steps to protect your reproductive health and seek appropriate medical care if necessary.
Causes of Spermatocele
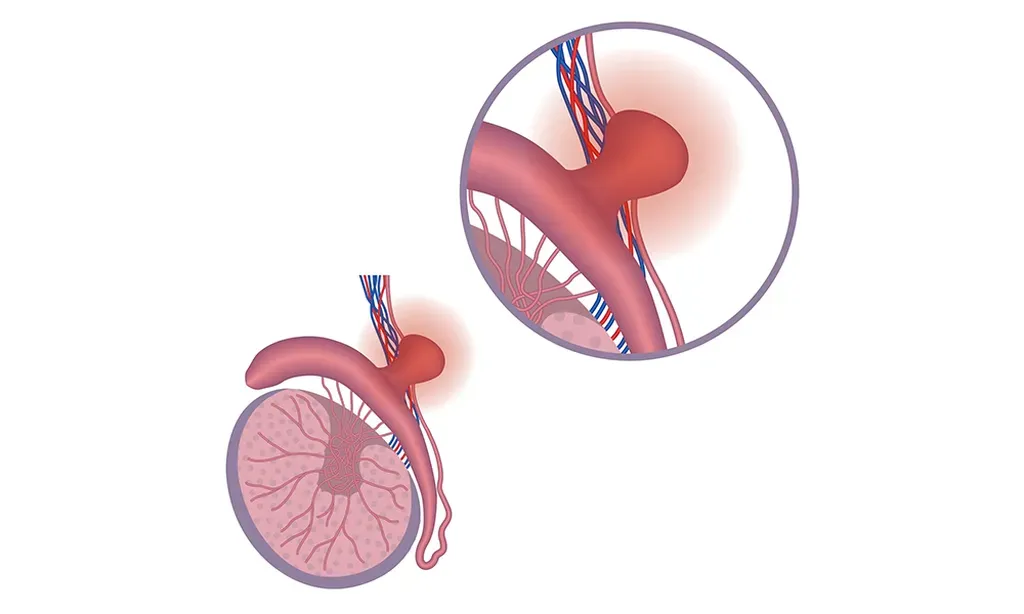
We still do not know the exact cause of spermatoceles. However, it is believed that they result from a blockage in the tubes that transport sperm. The epididymis is a tightly coiled tube that lies behind each testicle and is responsible for storing and carrying sperm. When the epididymis becomes blocked, sperm can build up and form a cyst or sac, which is known as a spermatocele.
Spermatoceles can also be caused by injury or infection in the epididymis. Injuries to the epididymis can cause scarring and blockages, which can lead to the formation of a spermatocele. Infections can cause inflammation and swelling, which can also lead to blockages in the epididymis.
Certain lifestyle factors may also increase the risk of developing a spermatocele. These include smoking, heavy alcohol consumption, and a poor diet. Additionally, some medical conditions, such as cystic fibrosis, can increase the risk of developing spermatoceles.
It is important to note that spermatoceles are not caused by sexually transmitted infections (STIs) or other sexually transmitted diseases (STDs). However, certain STIs and STDs can cause epididymitis, which is inflammation of the epididymis and can lead to the formation of a spermatocele.
Spermatocele Symptoms
Spermatoceles often do not cause any symptoms and are usually discovered during a routine physical exam. However, if they do cause symptoms, they may include:
Testicular self examination can be done when you have testicular pain to see if you need to see a board certified urologist for an appointment. Larger spermatoceles may cause more noticeable symptoms and will be more apparent during a testicular self exam. If you experience any of these symptoms, you should consult a qualified urologist today.
Diagnosis of Spermatocele
Spermatoceles are usually diagnosed through a physical exam. Urologists typically use the following tests to confirm a diagnosis:
Transillumination
Transillumination involves your doctor shining a light through the scrotum. Moreover, the light shows if the lump is fluid-filled or solid — if it’s fluid, you have a spermatocele.
Ultrasound
Your doctor might refer you for an ultrasound scan if the transillumination test isn’t clear enough for a definite diagnosis. Moreover, Ultrasound creates moving images using high-frequency sound waves. It can help determine if you have a testicular tumor or scrotal problem.
If your doctor suspects that the lump may be cancerous, they may order additional tests, such as a blood test or biopsy, to rule out testicular cancer.
It is important to perform regular self-exams to detect any changes or abnormalities in the scrotum. If you notice any lumps or swelling, or experience any pain or discomfort, you should consult a doctor for further evaluation.
Spermatocele Treatment
Spermatoceles can be treated with two main options: medications and surgical procedures.
Medications for Spermatocele
If your spermatocele is causing pain, your doctor might recommend over-the-counter pain medications, such as acetaminophen (Tylenol, others) or ibuprofen (Advil, Motrin IB, others). These medications can help alleviate the discomfort associated with the cyst.
Spermatocele Surgery
If your spermatocele is large or causing significant discomfort, you could benefit from surgery. The procedure called spermatocelectomy happens on an outpatient basis. Under anesthetic, they make an incision in your scrotum and detach the spermatocele from your epididymis.
You can go home the same day and you might need to wear an athletic support filled with gauze afterward. This applies pressure to the wound and protects it. Using ice packs for 2-3 days helps reduce swelling. Moreover, you must return to Comprehensive Urology for a follow-up exam 1-2 weeks after surgery.
It doesn’t usually affect fertility. But sclerotherapy and surgery can damage your epididymis or the vas deferens at the end of the epididymis. Our skilled surgeons at Comprehensive Urology rarely encounter this problem, but it’s advised to consider storing some sperm in a sperm bank before the procedure for peace of mind.
In addition, Less common treatments include aspiration (removing fluid from the cyst with a needle) and sclerotherapy (injecting fluid that scars the spermatocele). While there are risks associated with any surgical procedure, spermatocelectomies are generally considered safe and effective. Your doctor can help you weigh the risks and benefits of this procedure to determine if it’s the right choice for you.
Untreated Spermatocele
If left untreated, a spermatocele may lead to potential complications such as:
It is important to consult a doctor if you experience any discomfort or pain in the scrotum. Early diagnosis and treatment can help prevent potential complications.
Spermatocele Prevention
Spermatoceles are often harmless and do not require treatment unless they cause discomfort or affect fertility. However, there are certain steps that can be taken to prevent the development of spermatoceles.
Lifestyle Changes
Maintaining a healthy lifestyle can help reduce the risk of developing spermatoceles. Here are some lifestyle changes that can be made:
Regular Check-ups
Regular check-ups with a healthcare provider can help detect spermatoceles early on. During a routine physical exam, a healthcare provider will check for any abnormalities in the scrotum and testicles. If a spermatocele is detected, the healthcare provider may recommend further testing or treatment if necessary.
In some cases, treatment may be necessary to manage symptoms or prevent complications. Treatment options may include pain medications, aspiration (draining the fluid from the cyst), or surgery to remove the cyst. However, it is important to discuss the risks and benefits of treatment with a healthcare provider before making a decision.
Frequently Asked Questions
Can a spermatocele be dangerous?
Spermatoceles are usually benign and not dangerous. However, if you notice any changes in the size or shape of the spermatocele, or if you experience pain, it is important to seek medical attention.
What is the difference between a spermatocele and testicular cancer?
Spermatoceles are noncancerous growths, while testicular cancer is a malignant tumor. Testicular cancer may cause pain or discomfort in the testicles, a lump or swelling, or a feeling of heaviness in the scrotum. If you are concerned about any lumps or changes in your testicles, it is important to see a healthcare provider for evaluation.
How are spermatoceles treated?
Spermatoceles do not usually require treatment unless they are causing discomfort or affecting fertility. If treatment is necessary, your healthcare provider may recommend surgery to remove the spermatocele.
Spermatocele vs Hydrocele
Spermatocele and hydrocele are two distinct conditions that affect the male reproductive system. While they can both cause swelling in the scrotum, there are significant differences between the two conditions.
Spermatocele vs Epididymal Cyst
Spermatocele and epididymal cyst are two common conditions that can occur in the epididymis, which is a tightly coiled tube located on the upper testicle that collects and transports sperm. While both conditions involve fluid-filled sacs, there are some key differences between them.
Spermatoceles are typically caused by a blockage in the epididymis, which prevents the normal flow of sperm and causes the sac to fill with fluid. Epididymal cysts, on the other hand, are caused by a buildup of fluid in the epididymis that is not related to sperm production.
Spermatoceles and epididymal cysts may cause similar symptoms, such as a painless lump in the testicle or scrotum. However, spermatoceles are more likely to cause discomfort or pain than epididymal cysts. Additionally, spermatoceles may grow larger over time, while epididymal cysts typically remain the same size.
Both spermatoceles and epididymal cysts can be diagnosed through a physical examination and imaging tests, such as ultrasound. However, it can be difficult to differentiate between the two conditions based on imaging alone.
Spermatoceles and epididymal cysts may not require treatment if they are not causing any symptoms. However, if the sacs are causing discomfort or pain, or if they are growing larger over time, treatment may be necessary. Treatment options may include draining the fluid from the sac, removing the sac surgically, or monitoring the sac over time to ensure that it does not grow or become cancerous.
Spermatocele vs Varicocele
Spermatocele and varicocele are two separate urological conditions that can impact fertility, however Spermatocele is a cyst on the epididymis and varicocele is a varicose vein connected to the testicles.
A spermatocele is a cyst that forms in the epididymis, the small tube that collects and transports sperm from the testicles. It is usually filled with clear or milky fluid that may contain sperm. A varicocele, on the other hand, is a swelling of the veins that drain the testicles. It is often described as feeling like a “bag of worms” and can cause discomfort or pain.
One key difference between the two is the location of the swelling. Spermatoceles usually occur on the head of the epididymis, while varicoceles are typically found higher up, near the testicle itself. Additionally, while spermatoceles are usually painless, varicoceles can cause pain or discomfort, particularly when standing or exerting oneself.
Another difference is in their causes. Spermatoceles are often idiopathic, meaning they have no known cause. Varicoceles, on the other hand, are usually caused by a malfunctioning valve in the veins that causes blood to pool and swell the veins.
Both conditions can be diagnosed through a physical exam, ultrasound, or MRI. Treatment options for spermatoceles are typically only necessary if they are causing discomfort or affecting fertility. Varicoceles, on the other hand, may require treatment to relieve pain or improve fertility.
Spermatocele vs Testicular Cancer
Spermatoceles and testicular cancer are two conditions that can have similar symptoms which is why seeing a urologist is recommended to get a proper diagnosis and treatment.
Testicular cancer is a type of cancer that starts in the testicles and is often discovered when a patient notices a painless lump or swelling in the scrotum. Other symptoms such as pain or discomfort. Testicular cancer is relatively rare, but it is important to seek medical attention if you notice any changes in your testicles.
Differences between Testicular Cancer vs Spermatocele
Key differences between spermatoceles and testicular cancer:
It is important to note that while spermatoceles are not cancerous, they can sometimes be mistaken for testicular cancer. If you notice any changes in your testicles, it is important to see a board certified urologist as soon as possible.
What causes spermatoceles?
The exact cause of spermatoceles is not clear. However, it is believed that they may be due to a blockage in one of the tubes that transport sperm. Spermatoceles are also more common in men who have had a vasectomy.
How are spermatoceles diagnosed?
Spermatoceles are usually diagnosed during a physical examination. Your healthcare provider may also order an ultrasound to confirm the diagnosis.
What are the symptoms of a spermatocele?
Spermatoceles are often painless and do not cause any symptoms. However, some men may experience discomfort or a feeling of heaviness in the scrotum.
Sometimes our male patients who are already undergoing a medical procedure choose to also try a cosmetic procedure such as Scrotox to smooth out the wrinkles of the scrotum, scrotoplasty to address low hanging testicles, or penile injections to enhance girth. Schedule your appointment today to explore the options.




You must be logged in to post a comment.